Histamine, Salicylate and Sulphite Intolerance
Is There a Connection?
Margaret Moss, CBiol, MRSB, MA (Cantab)
When I started working in nutrition, people often came to me saying they had candida or leaky gut. Nowadays they often say they have histamine and salicylate intolerance, or they have Mast Cell Activation Syndrome, or small intestinal bacterial overgrowth. I suspect they are mostly the same kind of people, but descriptions vary over time. We’ve long known that Caesareans, bottle feeding, antibiotic abuse, low fat high sugar diets and NSAID abuse contribute to gut dysbiosis, both bacterial and fungal, and to leaky guts. I suspected my clients’ problems often related to sulphation, and we found, in our study of 81 of my patients, that none had normal results [1].
Leaky guts are usually sorted with sulphate, which attaches to the glycosaminoglycans of the gut lining, and with butter for butyric acid and coconut oil for lauric and myristic acid. Heating coconut oil gently releases volatile chemicals, and so the tasteless coconut oil is often better tolerated than the tasty one. It used to be thought that caprylic acid was the important part of coconut oil, but actually these other fatty acids are more important. I avoid using L-glutamine for leaky guts, as it quickly converts to glutamic acid, which is toxic to the brain. Lectins, in the bran layer of seeds, damage the gut, and bran, wholemeal bread, and pulses and nuts with skins contain plenty of lectins. Glucose is efficiently taken from the gut into the bloodstream, but fructose in fruit, sugar and honey, and galactose in milk are not so efficiently transported, and tend to linger in the gut, feeding unwanted microorganisms. Good quality probiotics, including L. Acidophilus and Bifido bacteria compete with harmful microorganisms, but avoid L. Rhamnosus, which has occasionally been linked to heart infections [2,3].
We make sulphate from cysteine, and a high ratio of cysteine x 1000 to sulphate suggests inefficiency at making sulphate. The ratio should be no more than 100. In our study, we found these average figures:
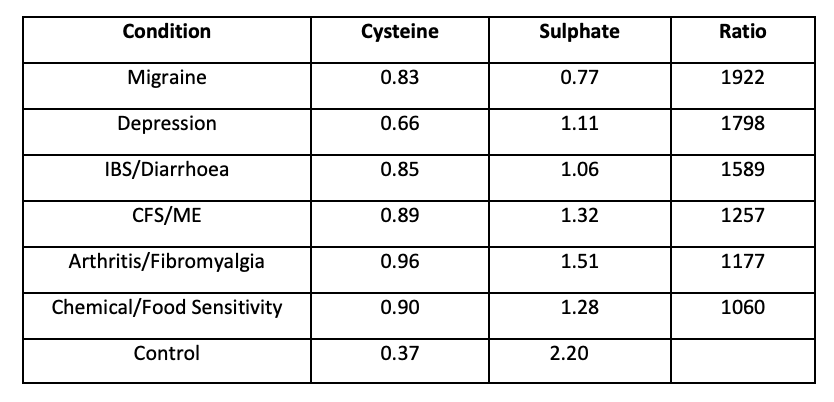
We are not looking at the tail of a normal distribution. We are looking at a bimodal distribution, with these chronic sick patients quite separate from the norm. The average cysteine for each condition is high. The average sulphate is low. The average ratio is far above the norm. These people are not typical, and normal public health advice does not apply to them.
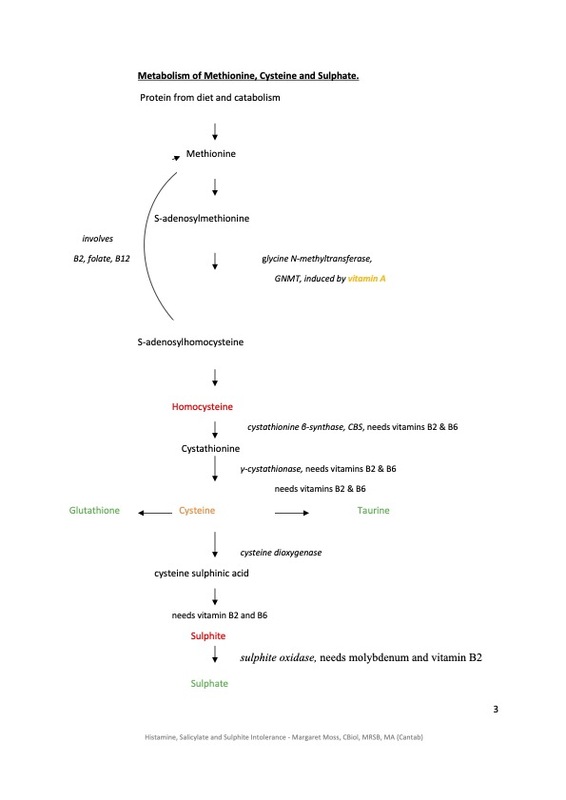
Does sulphate have other functions? Yes indeed. It detoxifies phenols, which are in foods, drugs, herbs and in the environment. We need sulphate to protect us from carcinogens, including oestrogen. Salicylates are phenols. Sulphate also detoxifies amines, which are in various foods, especially fermented or aged foods. It is needed to make hydrochloric acid and digestive enzymes, and also to activate cholecystokinin, which tells us when we have eaten enough. To improve the production of sulphate, we need to look at the biochemistry. In the diagram, I have coloured helpful chemicals in green, harmful ones in red, and ones that have good and bad effects in orange. Glutathione is very important for detoxification and reducing oxidative stress, taurine is calming, and reduces blood pressure. Cysteine acts against viruses, but overexcites nerve cells. Vitamin A is needed for immunity and vision, but is toxic in excess. It increases homocysteine production, which is why it is involved in neural tube defects, heart attacks and strokes. Sulphite, from food additives or coal smoke, can provoke asthma. It is listed in the Foods Standards Agency list of common allergens, but is a toxin rather than an allergen. Helpful nutrients are vitamin B6, vitamin B2 which activates B6, and is needed to make sulphate and energy and to recycle glutathione, and molybdenum, which is needed for several enzymes.
It is not enough to make sulphate. We need to transport it to where it is needed, using phenolsulphotransferase enzymes (SULT). Unfortunately, many vegetables and fruits inhibit this transport, especially spinach, radish and orange.
Our capacity to detoxify with sulphate is limited. We have a back-up mechanism to deal with phenols, which is glucuronidation. Those with poor glucuronidation are said to have Gilbert’s. They can be treated with calcium D glucarate. Gilbert’s is often seen as harmless. The problem comes if you have poor sulphation together with Gilbert’s. Your detoxification of phenols will be poor.
Histamine can be detoxified by sulphation. It can also be processed with methylation, the donation of a methyl group from S-adenosyl methionine. Homocysteine is removed by two pathways. One leads to sulphate. The other uses methylenetetrahydrofolate reductase (MTHFR), a vitamin B2 dependent enzyme, followed by either folate or synthetic folic acid, and then vitamin B12, to reconstitute methionine. Histamine is also removed by histaminase, or diamine oxidase, a copper enzyme. Copper rises in pregnancy, and some sensitive women feel much better when pregnant. If copper is deficient, you may be able to increase DAO levels simply with copper, without supplementing DAO itself.
Detoxification needs a lot of energy. Key nutrients for energy production are vitamin B2, vitamin B3, vitamin B5, which is also needed for making cortisol, and ubiquinol.
In some quarters it is fashionable to deal only with methylation. In others, only DAO is used. In others, people are told they are sensitive to sulphur. Sulphur is essential to life, but as with carbon, there are harmful sulphur compounds. In other quarters, people are told they need quercetin, as a mast cell stabiliser. The problem with this is that it is a phenol, and uses up our limited capacity for sulphation, thus leading to more issues with amines, phenols and too permeable guts.
It is important to understand sulphation, methylation and glucuronidation, as they are involved in many of the chronic health conditions of our times.
Questions and Answers
You mention that many have problems of low sulphate?
How important is adding in extra sulphate as in Epsom salt baths or sulphur containing vegetables or do you have other suggestion to increase sulphate?
It is very important to use Epsom salt baths, and I recommend 1 cupful of Epsom salts in the bath, 1 day in 3. I also recommend 400-500mcg of molybdenum, 25-100mg of riboflavin and 250-500mg of pantothenic acid a day, to increase the production of sulphate from sulphur amino acids in the diet. There is no need to increase the sulphur intake. I also suggest eating fish three times a week; or taking 3000mg of not concentrated fish oil a day; or occasional fish with a smaller dose of fish oil. Of course you should avoid farmed fish and tuna, to avoid toxins. Avoid concentrated fish oil, as the processing may damage it. The dose I have given is for the total oil, and not for eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA). These are specific omega three fats. You do not need 3000mg of EPA + DHA. I do not advocate cod liver oil, as the vitamin A dose in it is too high. Omega 3 and 6 fatty acids are both essential, and the intake should be balanced. Nuts and seeds provide omega 6. I warn my patients that prescriptions are not forever, and may need to be revised later.
I am struck by the importance of sulphate for digestion. Are stomach acid problems or being on a PPI a red flag for a sulphate problem?
If someone has low stomach acid due to poor sulphation, then using a PPI will make matters worse.
Do we need to avoid or reduce the amount of aspirin or quercetin in patients with Gilberts?
Aspirin and quercetin are phenols, which are processed using sulphation and glucuronidation. It would make sense to avoid these in Gilbert’s patients, and it is even more important to avoid them if there is also a sulphation issue.
The cysteine/sulphate ratios were simply astonishing, especially in migraine and depression. Do you have clinical evidence that supplementing B vitamins and molybdenum make a difference as biochemically they should do in these conditions?
I use a combined approach, with supplements, diet and lifestyle advice. Clinical audit shows that that works. I do not use supplementation alone. I expect it would be less effective. Patients do report that running out of their supplements causes deterioration, as does breaking the diet. One ME patient twice rang me the evening before travelling abroad. She had counted her molybdenum tablets, and realised she did not have enough. Please could she drive over that evening to collect some from me, as she could not go away without them? She lived a significant distance away.
In people with too much histamine it appears there is likely to be a sulphation problem? Have you found that using B vitamins and copper has helped clinically as it should improve histamine breakdown?
Molybdenum, omega three fats, B2 and B5 help with sulphation. Magnesium, B2, folate and B12 help with methylation. Copper helps with histaminase (DAO). Ideally test for deficiencies. Functional B2 is often poor.
There has been some worries about coconut oil being converted into the inflammatory compound TMAO. Is this a concern?
The main concern with trimethylamine-N-oxide (TMAO) is with fish, but omega three fatty acids are so important that I encourage fish consumption. I am much more concerned at the amount of inflammatory omega six fats people consume. These fats are essential, but often consumed excessively, and they are damaged by harsh oil processing and by frying. Incidentally, these damaged oils are thought to contribute to the cytokine storm seen in some Covid-19 patients. TMAO is thought to be a risk factor for coronary heart disease, but CHD is a disease of milk drinkers, not those living amongst coconut palms [4,5,6].
You mention in the full article about fish oils and low protein diet. How important are these?
Fish or fish oil is important. I do not advocate a low protein diet, except if there is a relevant inborn error of metabolism, but cysteine is an excitotoxic amino acid, and the current fashion for prescribing N-acetyl cysteine (NAC) without testing cysteine levels is very worrying. It is however very useful in AIDS and paracetamol poisoning.
Is there a way we could measure cysteine levels?
Cysteine and sulphate levels used to be measured at Birmingham University, but this is no longer available. Biolab used to do a group of amino acids, but only in urine. Cysteine levels in plasma should be measured as close to 8 a.m. as possible. Amino acid levels will vary through the day.
References
1. Moss M, Waring RH. The Plasma Cysteine/Sulphate Ratio: a Possible Clinical Biomarker. J Nutr Env Med 2003; 13(4): 215-229.
2. Campagne J, Guichard JF, Moulhade MC, Kawski H, Maurier F. Lactobaciollus endocarditis: a case report in France and literature review. ID Cases 2020; 21:e00811.
3. Rossi F, Amadoiro C, Gasperi M, Colavita G.Lactobacilli Infection Case reportsdin the last three years and safety implications. Nutrients 2022; 14(6):1178.
4. Moss M, Freed DLJ. Survival Trends, Coronary Event Rates, and the MONICA Project (letter). Lancet 1999; 354 (9181): 862.
5. Moss M. Does Milk Cause Coronary Heart Disease? J Nutr Env Med 2002; 12(3): 207-16.
6. Moss M, Freed D. The Cow and the Coronary: Epidemiology, Biochemistry and Immunology. Int J Cardiol 2003; 87: 203-216.